Starting with the launch of the Human Genome Project three decades ago, and continuing after its completion in 2003, genomics has progressively come to have a central and catalytic role in basic and translational research.
In addition, studies increasingly demonstrate how genomic information can be effectively used in clinical care.
In the future, the anticipated advances in technology development, biological insights, and clinical applications (among others) will lead to more widespread integration of genomics into almost all areas of biomedical research, the adoption of genomics into mainstream medical and public-health practices, and an increasing relevance of genomics for everyday life.
On behalf of the research community, the National Human Genome Research Institute recently completed a multi-year process of strategic engagement to identify future research priorities and opportunities in human genomics, with an emphasis on health applications.
This decrease has allowed the generation of innumerable genome sequences, including hundreds of thousands of human genome sequences (both in research and clinical settings), and the continuous development of assays to identify and characterize functional genomic elements5,61
In turn, the past decade has brought the initial realization of genomic medicine11, as research successes have been converted into powerful tools for use in healthcare, including somatic genome analysis for cancer (enabling development of targeted therapeutic agents)12, non-invasive prenatal genetic screening13, and genomics-based tests for a growing set of paediatric conditions and rare disorders14, among others.
In essence, with growing insights about the structure and function of the human genome and ever-improving laboratory and computational technologies, genomics has become increasingly woven into the fabric of biomedical research, medical practice, and society.
The scope, scale, and pace of genomic advances so far were nearly unimaginable when the Human Genome Project began; even today, such advances are yielding scientific and clinical opportunities beyond our initial expectations, with many more anticipated in the next decade.
Embracing its leadership role in genomics, the National Human Genome Research Institute (NHGRI) has developed strategic visions for the field at key inflection points, in particular at the end of the Human Genome Project in 200315 and then again at the beginning of the last decade in 2011162
These visions outlined the most compelling opportunities for human genomics research, in each case informed by a multi-year engagement process.
NHGRI endeavoured to start the new decade with an updated strategic vision for human genomics research.
During the Human Genome Project, NHGRI was the primary funder of human genomics research at the US National Institutes of Health (NIH), but the past two decades have brought a greater than tenfold increase in the relative fraction of funding coming from other parts of the NIH.
Also shown (bottom) is the relative proportion of funds supporting human genomics research provided by NHGRI versus all of the NIH for the three corresponding time intervals (as derived from queries of the internal NIH Research, Condition, and Disease Categorization database for funds assigned to the ‘human genome’ category).
During the 30-year period when the NHGRI budget increased roughly tenfold (middle), the proportion of total NIH funding for human genomics research actually increased more markedly, from less than 5% during the Human Genome Project to around 90% at the beginning of the current decade (bottom).
In essence, these trends reflect a leveraging of NHGRI’s funds that increased NIH’s overall human genomics research funding by greater than tenfold.
• Maintain an overarching focus on using genomics to understand biology, to enhance knowledge about disease, and to improve human health — genomics is now foundational across the entire continuum of biomedical research, from deciphering fundamental principles of biology to translating that knowledge into disease prevention and medical advances.
• Strive for global diversity in all aspects of genomics research, committing to the systematic inclusion of ancestrally diverse and underrepresented individuals in major genomic studies — attention to diversity in genomics research is both socially just and scientifically essential, which includes meaningful, sustained partnerships with diverse communities in the design and implementation of research studies, the propagation of research findings, and the development and use of new technologies.
• Provide a conceptual research framing that consistently examines the role of both genomic and non-genomic contributors to health and disease — routinely considering the importance of social and environmental factors that influence human health (and the interactions among those components and genomics) will be important for the comprehensive understanding of most human diseases.
• Promote robust and consistently applied standards in genomics research — the use of carefully defined standards (for example, those for generating, analysing, storing, and sharing data) has benefited genomics in numerous ways, and this must include appropriate privacy and data-security protections for those participating in genomics research.
• Embrace the interdisciplinary and team-oriented nature of genomics research — starting with the Human Genome Project, some of the most challenging genomics endeavours have benefited from the creation and management of large, interdisciplinary research collaborations.
• Adhere to the highest expectations and requirements related to open science, responsible data sharing, and rigor and reproducibility in genomics research — the genomics enterprise has a well-respected history of leading in these areas, and that commitment must be built upon and continually reaffirmed.
• Enable the routine generation and analysis of increasingly complex genomic data.
• Use evolutionary and comparative genomic data to maximize understanding of genome function.
Genomic data science.
• Develop new methods and build sustainable data resources for genomics research.
• Develop integrated knowledgebases and informatics methods for genomic medicine.
• Empower people to make well-informed decisions about genomic data and develop data-stewardship systems that reinforce their choices.
• Ensure that the next generation of genomic scientists are sufficiently trained in data science.
• Develop and assess strategies for implementing the use of genomic information in clinical care.
• Design studies that include diverse ancestral populations to enable scientific discoveries and genomic medicine for all.
• Design and use genomic learning healthcare systems for knowledge generation and improvements in clinical care.
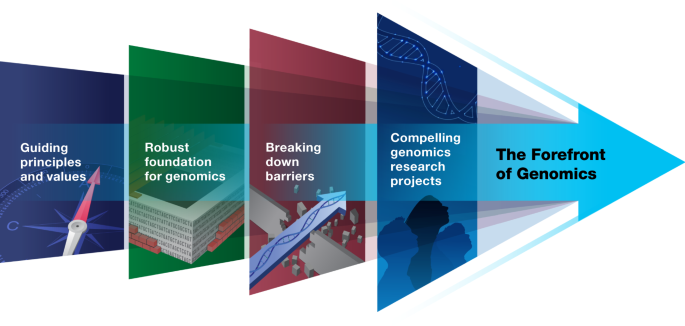
The growing complexities of human genomics and its many applications (especially in medicine) at The Forefront of Genomics make it imperative to reaffirm, sharpen, and even extend these tenets, such as those highlighted in Box 1.
Many of these principles and values have been informed by the recognized area of genomics that focuses on ethical, legal, and social implications (ELSI) research17, which was established at the beginning of the Human Genome Project to ensure that the eugenics movement and other misuses of genetics are not repeated.
ELSI research has since grown to encompass a broad portfolio of studies that examine issues at the interface of genomics and society, the results of which have informed policies and laws related to genetic discrimination, intellectual property, data sharing, and informed consent18.
In the future, ELSI research needs to focus on aspects of genomic medicine implementation that present challenging questions about legal boundaries, study governance, data control, privacy, and consent.
Finally, ELSI research should also examine the implications of studying genetic associations with bio-behavioural traits (such as intelligence, sexual behaviour, social status, and educational attainment)21 and of a future in which machine learning and artificial intelligence are used to adapt risk communication and clinical decisions based on analysing an individual’s genome sequence22.
Genomics is now routinely and broadly used throughout biomedical research, with widespread reliance on a robust foundation for facilitating genomic advances.
Further opportunities are anticipated as the generation and analysis of genomic data become even faster, cheaper, and more accurate.
These genomic data should be integrated with other multi-omic data (for example, proteomes, metabolomes, lipidomes, and/or microbiomes) in sophisticated ways, including methods that collect many data types from a single sample32.
Transformative approaches will become increasingly vital for assimilating, sharing, and analysing these complex and heterogeneous data types33 and must expand to include the integration of environmental, lifestyle, clinical, and other phenotypic data.
Understanding natural genomic variation, the conservation of genomic elements, and the rapid evolutionary changes in genomic regions associated with specific traits is crucial for attaining a comprehensive view of genome structure and function.
The study of a wide range of organisms continues to be instrumental for determining the effect of genomic variation on biological processes and phenotypes, providing insights about the interplay of genomic variants and environmental pressures35 and the relevance of putative pathogenic variants identified in clinical studies36.
It is essential that the generation of high-quality multi-species genomic data is accompanied by community-accepted standards for data, metadata, and data interoperability.
New methods would allow for integrating functional data from diverse species with human data and visualizing increasingly complex comparative genomic datasets.
Furthermore, the biomedical research community requires accurate, curated, accessible, secure, and interoperable genomic data repositories and informatics platforms that benefit all populations.
Recent progress has brought substantial transformations in how the petabytes of genomic data being generated each year are assimilated and analysed, including the emergence of cloud-based and federated approaches.
Current barriers include the lack of interoperable genomic data resources (which limits downstream access, integration, and analyses) and the absence of controlled and consistently adopted data and metadata vocabularies and ontologies41,42.
The full integration of genomics into medical practice will require informatics and data-science advances that effectively connect the growing body of genomic knowledge to clinical decision-making.
To make genomic information readily accessible and broadly useful to clinicians, user-friendly electronic health record-based clinical decision support tools must be created to interact with a variety of clinical data from electronic health record and other data systems (for example, laboratory, pharmacy, and radiology) as well as non-computable reports, such as those provided as portable document format (PDF) files43,44.
These efforts require well-curated, highly integrated, and up-to-date knowledgebases that connect genomic information to clinical characteristics, other phenotypic data, and information on family health history45.
Reliable risk-stratification and prevention algorithms, including polygenic risk scores (PRSs)46, must be developed and should incorporate both common and rare genomic variants from a broad range of population subgroups, phenotypic data, and environmental information into the risk modelling47.
Understanding the role of genomics in human health requires knowledge and insights about how social, environmental, and genomic risk factors interact to produce health outcomes48,49 (Box 1).
Optimal implementation of genomic medicine will require an understanding of how the intersectional aspects of people’s social and political identities influence the ways in which populations are described in research.
People want to be able to make well-informed decisions about their genomic data, leading to the engagement efforts in initiatives such as the UK Biobank52 and the ‘All of Us’ Research Program53.
Furthermore, given the ever-expanding use of genomics in basic, translational, social, behavioural, and clinical research, a greater number of scientists will require fundamental data-science skills that are appropriate for the genomic applications being used66.
Establishing and maintaining data-science competencies for conducting genomics research requires a series of interrelated educational and training efforts67, including the recruitment of many data scientists into genomics and the reciprocal exchange of expertise between genomics researchers and data scientists.
In both research and clinical settings, the global genomics workforce—as with the general biomedical research workforce—falls considerably short of reflecting the diversity of the world’s population (a vivid example of this is seen in the United States72), which limits the opportunity of those systematically excluded to bring their unique ideas to scientific and clinical research73.
Prototypic successes include the call for a ‘[US]$1,000 human genome sequence’ after completion of the Human Genome Project15 and proposed actions to facilitate genomic medicine implementation in 201116; in these cases, both the risks of failure and the benefits of success were high.
Once again, breaking down barriers, as highlighted in Box 3 and detailed below, would accelerate progress and create new research and clinical opportunities at The Forefront of Genomics.
Genome editing is increasingly being used for practical applications in medicine (such as in gene therapy76), biotechnology, and agriculture.
Despite recent triumphs, however, the current approaches are limited in their ability to interrogate genome function at the pathway or network level and to study important phenomena, such as gene regulation and chromosome organization and mechanics, that involve factors that act across large chromosomal (or genomic) distances.
Furthermore, radically new capabilities for understanding how the full complement of genomic variation within any individual genome contributes to phenotype should be pursued.
In recent years, large human genomics projects have often relied on data generated as part of existing research studies, and emerging approaches involve developing biobanks and organized cohorts77,78,79.
Meanwhile, DTC companies are generating substantial amounts of genomic data, and those efforts are rapidly being eclipsed by that being generated in the clinical care setting80.
Properly leveraged, these DTC and clinical data offer opportunities for genomics-based studies at unprecedented scales; however, these data are often heavily fragmented, siloed, and mostly outside the purview of genomics researchers and their typical funders81.
The cycle on the left reflects basic genomics research, in which technology innovations spur the collection and analysis of genomics research data, often yielding new knowledge and further hypotheses for testing?
The cycle on the right reflects a genomic learning healthcare system, in which the implementation of new genomic medicine practice innovations allows for the collection and analysis of outcomes data, often yielding new genomic knowledge and additional genomics-based strategies for improving the quality of clinical care.
Progress in this area requires global collaboration85, advances in integrating several data types and performing perturbation assays, protein localization or interaction experiments, and animal models, as well as resources cataloguing information about the fitness consequences of de novo mutations and the clinical relevance of genomic variants83.
Important areas of future research include investigating the prevalence and extent of different forms of mosaic variation in both nuclear and mitochondrial DNA, the mechanisms that generate mosaicism, and the roles of mosaicism in physiology and human disease.
The development of laboratory and clinical approaches to readily detect genomic mosaicism at high spatial and temporal resolutions, especially in non-invasive ways (for example, requiring minimal amounts of tissue), would be catalytic.
A crucial barrier to using genomics for improving health and preventing disease is the lack of clinical uptake of proven genomic interventions.
Implementation science approaches are needed to identify the most effective methods and strategies for facilitating the use of evidence-based genomic applications, most notably pharmacogenomics-based selection of medications90, in routine clinical care.
The effectiveness of centralized resources for genomic referrals (for example, genomic medicine specialists, consult services93,94, and centres of excellence in undiagnosed diseases—akin to transplantation centres or cancer centres) should be explored as potential steppingstones to the more generalized uptake of genomics in clinical care.
New methods to analyse data that account for human diversity103, coupled with a growing clarity about genotype–phenotype relationships, must be developed to deduce associations and interactions among genomic variants and environmental factors, improve estimates of penetrance and expressivity, and enhance the clinical utility of genomic information for predicting risk, prognosis, treatment response, and, ultimately, clinical outcomes.
Prioritizing the generation of genomic and corresponding phenotypic data from ancestrally diverse participants is a scientific imperative104 and essential for achieving equitable benefits from genomic advances105 (Box 1).
However, this is an area in which genomics has repeatedly fallen short19, leading to missed opportunities for understanding genome structure and function, identifying variants conferring risk for common diseases106, and implementing genomic medicine for the benefit of all107,108,109.
Success in these efforts will yield a more-complete understanding of how the human genome functions in different environments and offer benefit to those participating in genomics research.
Research that catalogues, analyses, and measures the effect of genomics on individuals, families, and communities is important to provide a more informed context to avoid future misrepresentations, misunderstandings, and misuses of genomics54.
Extending genomics research in clinical settings beyond DNA sequence to include other multi-omic data, together with clinical variables and outcomes, would advance understanding of disease onset and progression and may also prove important for drug-discovery efforts113,114.
For clinical applicability and adoption, these high-dimensional, multi-omic data should be integrated with clinical decision support tools and electronic health records.
Ultimately, such efforts could reveal important relationships among genomic, environmental, and behavioural variation and facilitate a transition of the use of genomics in medicine from diagnosing and treating disease to maintaining health.
Learning healthcare systems—in which real-time data on outcomes of healthcare delivery are accessed and used to enhance clinical practice—can lead to continuous care improvement, but only if the barriers between research and clinical care are reduced115.
For example, offering genome sequencing to all members of a healthcare system, performed in conjunction with research and participant engagement and provided in real time81, could help to assess the clinical utility of genomic information and may allow providers to improve disease diagnosis and management.
System-wide implementation of such an experiment requires not only extensive patient and provider education, sophisticated informatics capabilities, and genomics-based clinical decision support, but also the development and evaluation of data security and privacy protections to ensure patient confidentiality116.
Patients should be engaged in the design of such systems and informed at entry to them (and periodically thereafter), so as to be fully aware of the nature of the ongoing research with their clinical data and the goals and potential risks of their participation117.
Extending such studies across many healthcare systems should reveal common challenges and solutions118,119, thereby enhancing the learning healthcare model for genomic medicine more broadly (Fig. 3).
The dawn of genomics featured the launch of the Human Genome Project in October 19901.
Three decades later, the field has seen stunning technological advances and high-profile programmatic successes, which in turn have led to the widespread infusion of genomic methods and approaches across the life sciences and, increasingly, into medicine and society.
NHGRI has for the third time15,16 since the Human Genome Project undergone an extensive horizon-scanning process to capture, synthesize, and articulate the most compelling strategic opportunities for the next phase of genomics—with particular attention to elements that are most relevant to human health.
Another reality was that the NHGRI investment in genomics has now been multiplied many-fold by the seeding of human genomics throughout the broader research community.
Major unsolved problems remain—among them determining the role for the vast majority of functional elements in the human genome (especially those outside of protein-coding regions), understanding the full spectrum of genomic variation (especially that implicated in human disease), developing data-science capabilities (especially those that keep pace with data generation), and improving healthcare through the implementation of genomic medicine (especially in the areas of prevention, diagnosis, and therapeutic development).
Towards that end (and with the characteristic spirit of genomics audacity), we offer ten bold predictions of what might be realized in human genomics by 2030 (Box 5).
The strategic vision articulated here was crafted on behalf of the field of human genomics and emphasizes broad strategic goals as opposed to implementation tactics.
In concluding NHGRI’s previous strategic vision16—published just under a decade ago —the then-envisioned opportunities and challenges were provided with “… a continuing sense of wonder, a continuing need for urgency, a continuing desire to balance ambition with reality, and a continuing responsibility to protect individuals while maximizing the societal benefits of genomics….†With the 2020 strategic vision described here providing a thoughtful guide and with enduring feelings of wonder, urgency, ambition, and social consciousness providing unfettered momentum, we are ready to embark on the next exciting phase of the human genomics journey.
Here are ten bold predictions for human genomics that might come true by 2030.
Generating and analysing a complete human genome sequence will be routine for any research laboratory, becoming as straightforward as carrying out a DNA purification.
The biological function(s) of every human gene will be known; for non-coding elements in the human genome, such knowledge will be the rule rather than the exceptionD
Research in human genomics will have moved beyond population descriptors based on historic social constructs such as race.
Studies that involve analyses of genome sequences and associated phenotypic information for millions of human participants will be regularly featured at school science fairs.
The regular use of genomic information will have transitioned from boutique to mainstream in all clinical settings, making genomic testing as routine as complete blood counts.
The clinical relevance of all encountered genomic variants will be readily predictable, rendering the diagnostic designation ‘variant of uncertain significance (VUS)’ obsoleteJ
Individuals from ancestrally diverse backgrounds will benefit equitably from advances in human genomics.
Genomics rapidly assumed crucial roles in COVID-19 research and clinical care in areas such as (1) the deployment of DNA- and RNA-sequencing technologies for diagnostics, tracking of viral isolates, and environmental monitoring; (2) the use of synthetic nucleic acid technologies for studying SARS-CoV-2 virulence and facilitating vaccine development; (3) the examination of how human genomic variation influences infectivity, disease severity, vaccine efficacy, and treatment response; (4) the adherence to principles and values related to open science, data sharing, and consortia-based collaborations; and (5) the provision of genomic data science tools to study COVID-19 pathophysiology.
The growing adoption of genomic approaches and technologies into myriad aspects of the global response to the COVID-19 pandemic serves as another important and highly visible example of the integral and vital nature of genomics in modern research and medicine.
The Human Genome Project; https://www.genome.gov/human-genome-project (accessed 28 June 2020).
Initial sequencing and analysis of the human genome.
PubMed Central A
International Human Genome Sequencing Consortium.
Finishing the euchromatic sequence of the human genome.
The cost of sequencing a human genome; https://www.genome.gov/about-genomics/fact-sheets/Sequencing-Human-Genome-cost (accessed 12 June 2020).
PubMed Central W
PubMed Central .
Analysis of a large dataset of exome sequences, yielding important descriptions of the extent and nature of human genomic variation and insights into protein evolution.
PubMed Central .
PubMed Central S
PubMed Central S
PubMed Central .
PubMed Central .
PubMed Central .
PubMed Central .
PubMed Central B
Charting a course for genomic medicine from base pairs to bedside.
PubMed Central .
The Ethical, Legal, and Social Implications Program of the National Human Genome Research Institute: reflections on an ongoing experimentI
PubMed Central .
PubMed Central .
Integrating rules for genomic research, clinical care, public health screening and DTC testing: creating translational law for translational genomics.
PubMed Central .
Artificial intelligence in clinical and genomic diagnostics.
PubMed Central .
Cultivating DNA sequencing technology after the human genome project.
PubMed Central .
PubMed Central .
PubMed Central .
PubMed Central L
PubMed Central .
PubMed Central .
PubMed Central .
Biological data sciences in genome researchC
PubMed Central .
Description of foundational principles to improve data sharing and stewardship by ensuring that biomedical research data (including genomic data) are findable, accessible, interoperable, and reusable.
PubMed Central .
Data lakes, clouds, and commons: a review of platforms for analyzing and sharing genomic data.
PubMed Central .
PubMed Central .
Opportunities to implement a sustainable genomic medicine program: lessons learned from the IGNITE Network.
Genomic information for clinicians in the electronic health record: Lessons learned from the clinical genome resource project and the electronic medical records and genomics network.
PubMed Central .
PubMed Central C
PubMed Central .
PubMed Central .
Google Scholar J
PubMed Central .
The UK Biobank resource with deep phenotyping and genomic data.
PubMed Central .
PubMed Central .
Google Scholar .
Discussion of issues related to conducting genomics research with Indigenous peoples, coupled with suggestions for respecting tribal governance and protecting Indigenous people from group harms.
PubMed Central V
Google Scholar .
Google Scholar .
Trust in genomic data sharing among members of the general public in the UK, USA, Canada and Australia.
PubMed Central .
Google Scholar .
Data privacy in the age of personal genomics.
PubMed Central .
Google Scholar J
PubMed Central .
Google Scholar S
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central A
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar J
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
Development of an evidence-based, theory-informed national survey of physician preparedness for genomic medicine and preferences for genomics continuing education.
PubMed Central .
Google Scholar .
Challenges and opportunities for genomics education: Insights from an Institute of Medicine Roundtable Activity.
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
Synthetic genomics: a new venture to dissect genome fundamentals and engineer new functions.
PubMed Central J
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
Bedside back to bench: building bridges between basic and clinical genomic research.
PubMed Central .
Google Scholar A
ClinGen — The clinical genome resource.
PubMed Central .
Google Scholar .
PubMed Central K
Google Scholar .
PubMed Central .
Google Scholar .
Google Scholar .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
A clinical service to support the return of secondary genomic findings in human research.
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar S
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central A
Google Scholar .
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
Google Scholar .
Prioritizing diversity in human genomics research.
PubMed Central .
Google Scholar .
PubMed Central .
Google Scholar .
Lack of diversity in genomic databases is a barrier to translating precision medicine research into practice.
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
Successful recruitment and retention of diverse participants in a genomics clinical trial: a good invitation to a great party
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
Google ScholarÂ
International code of conduct for genomic and health-related data sharing
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
PubMed CentralÂ
Google ScholarÂ
A global collaborative to advance genomic medicine
PubMed CentralÂ
Google ScholarÂ
The National Advisory Council for Human Genome Research (current members are J. Botkin, T. Ideker, S. Plon, J. Haines, S. Fodor, R. Irizarry, P. Deverka, W. Chung, M. Craven, H. Dietz, S. Rich, H. Chang, L. Parker, L. Pennacchio, and O. Troyanskaya) ratified the strategic planning process, themes, and priorities associated with this strategic vision
National Human Genome Research Institute, National Institutes of Health, Bethesda, MD, USA