– Neurology research can include information involving brain research, neurological disorders, medicine, brain cancer, peripheral nervous systems, central nervous systems, nerve damage, brain tumors, seizures, neurosurgery, electrophysiology, BMI, brain injuries, paralysis and spinal cord treatments.
Our psychology articles cover research in mental health, psychiatry, depression, psychology, schizophrenia, autism spectrum, happiness, stress and more.
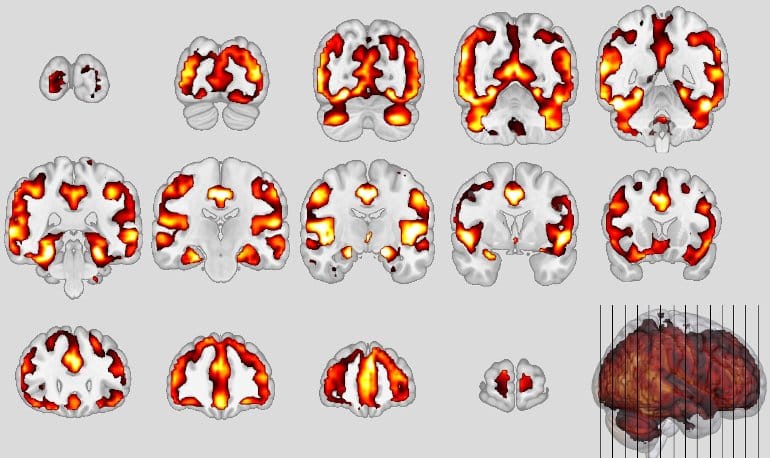
Summary: Study reveals striking similarities in both behaviors and neuroanatomical changes between people with schizophrenia and behavioral-variant frontotemporal dementia.Researchers have, for the first time, compared schizophrenia and frontotemporal dementia—disorders that are both located in the frontal and temporal lobe regions of the brain.But now, with the help of imaging and machine learning, scientists have found the first valid indications of neuroanatomical patterns in the brain that resemble the signature of patients with frontotemporal dementia.By the beginning of the 20th century, experts were beginning to use the term “schizophrenia” for these patients, since the disease does not take such a bad course in all persons concerned.Kraepelin had the idea of a frontotemporal disease, he assumed that the reason for the sometimes-debilitating course of the patients is located in the frontal and temporal lobe areas of the brain.Similarities between schizophrenia and frontotemporal dementia.Frontotemporal dementia (FTD), especially the behavioral variant (bvFTD), is difficult to recognize in its early stages because it is often confused with schizophrenia.The result, just published in the journal JAMA Psychiatry, was that 41% of schizophrenia patients met the classifier’s criteria for bvFTD.However, shared brain alterations remain disputed, and their relevance for patients in at-risk disease stages has not been explored so far.
To use machine learning to compare the expression of structural magnetic resonance imaging (MRI) patterns of behavioral-variant frontotemporal dementia (bvFTD), Alzheimer disease (AD), and schizophrenia; estimate predictability in patients with bvFTD and schizophrenia based on sociodemographic, clinical, and biological data; and examine prognostic value, genetic underpinnings, and progression in patients with clinical high-risk (CHR) states for psychosis or recent-onset depression (ROD).This study included 1870 individuals from 5 cohorts, including (1) patients with bvFTD (n = 108), established AD (n = 44), mild cognitive impairment or early-stage AD (n = 96), schizophrenia (n = 157), or major depression (n = 102) to derive and compare diagnostic patterns and (2) patients with CHR (n = 160) or ROD (n = 161) to test patterns’ prognostic relevance and progressionCase assignments based on diagnostic patterns; sociodemographic, clinical, and biological data; 2-year functional outcomes and genetic separability of patients with CHR and ROD with high vs low pattern expression; and pattern progression from baseline to follow-up MRI scans in patients with nonrecovery vs preserved recoveryThe bvFTD pattern comprising prefrontal, insular, and limbic volume reductions was more expressed in patients with schizophrenia (65 of 157 [41.2%]) and major depression (22 of 102 [21.6%]) than the temporo-limbic AD patterns (28 of 157 [17.8%] and 3 of 102 [2.9%], respectively)
The schizophrenia pattern was expressed in 92 of 108 patients (85.5%) with bvFTD and was linked to the C9orf72 variant, oligoclonal banding in the cerebrospinal fluid, cognitive impairment, and younger age (R2 = 0.29)
bvFTD and schizophrenia pattern expressions forecasted 2-year psychosocial impairments in patients with CHR and were predicted by polygenic risk scores for frontotemporal dementia, AD, and schizophrenia
Finally, 1-year bvFTD/schizophrenia pattern progression distinguished patients with nonrecovery from those with preserved recovery